Best Low FODMAP Foods for IBS
The best low FODMAP foods for IBS relief, along with additional nutritional strategies like fiber intake, probiotics, hydration, and key supplements that may help support gut health.
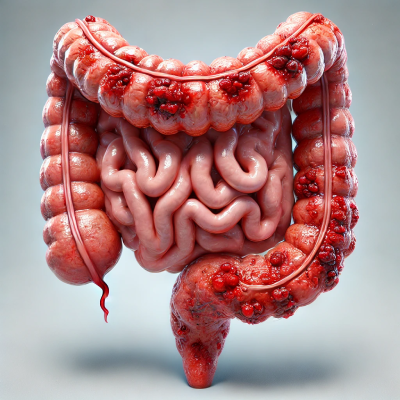
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder that affects millions of people worldwide. While there is no definitive cure, the good news is that IBS symptoms can be effectively managed through dietary and lifestyle modifications. One of the most evidence-based approaches is following a low FODMAP diet, which helps reduce bloating, gas, diarrhea, and constipation by eliminating certain fermentable carbohydrates.
IBS and the role of diet
Diet plays a crucial role in the control of IBS symptoms. Certain carbohydrates, known as FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols), are poorly absorbed in the small intestine, leading to intestinal fermentation and discomfort.
The low FODMAP diet consists of temporarily eliminating FODMAP-rich foods and then systematically reintroducing them to identify personal triggers.
Best Low FODMAP Foods for Symptom Relief
Low FODMAP foods are well tolerated and are a good choice for people with severe symptoms.
Here are some low FODMAP foods that are safe to include in your diet:
- Proteins: chicken, turkey, eggs, tofu, firm cheese (cheddar, parmesan) and most seafood.
- Vegetables: Carrots, zucchini (without skin), cucumbers and green beans.
- Fruits: Bananas (green), oranges, grapes, grapes, kiwis, strawberries, lemon, tangerine and blueberries.
- Cereals and starches: Rice, quinoa, oats and potatoes.
Including these foods can help prevent bloating and discomfort while ensuring balanced nutrition.
The Role of Soluble Fiber in IBS Management
Fiber is essential for digestion, but not all fiber is equal. Insoluble fiber (present in wheat bran and some raw vegetables) can be poorly tolerated by the gut, while soluble fiber helps regulate bowel movements and improve symptoms.
Examples of good sources of soluble fiber for IBS: oats, chia seeds, carrots and ripe bananas.
Adding these foods gradually can help prevent excessive fermentation, which can cause bloating.
Probiotics and IBS: Which Strains Actually Work?
The probiotic strains that have shown significant improvements either alone or in combination, mainly in flatulence and abdominal distension are: Bifidobacterium longum LA 101, Lactobacillus acidophilus LA 102, Lactococcus lactis LA 103 and Streptococcus thermophilus LA 104.
However, in my experience as a nutritionist, including natural sources of probiotics such as kefir yogurt can also help reduce symptoms despite the diversity of its strains.
Hydration and Digestive Health
Adequate hydration is essential to control the symptoms of irritable bowel syndrome. Dehydration can worsen constipation, while excessive consumption of carbonated or sugary drinks can cause bloating.
My recommendation is to consume 35 ml of water per kg of body weight, your intake can be through water or infusions (mint, ginger, chamomile).
On the other hand, avoid excessive consumption of caffeine, alcohol and artificial sweeteners, as they can irritate the intestine.
Best Low FODMAP Foods for IBS: Final tips
As a nutritionist, I recommend increasing consumption of low FODMAP foods, soluble fiber sources and adequate hydration to improve and prevent IBS symptoms. In addition, if necessary, probiotic supplements of specific or natural strains can be included.
However, depending on individual tolerance, it is necessary to progress to a food reintroduction phase to identify specific triggers.
As additional recommendations, prefer small, frequent meals to reduce intestinal overload.
Remember to keep a food diary to monitor symptoms and identify patterns.
In addition, stress plays a key role in symptom management.
If symptoms persist, consulting a nutritionist or dietitian can help you customize your approach.
Written by: Nutritionist Andrés Izurieta
Bibliographic citations:
Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. Lancet. 21 de noviembre de 2020;396(10263):1675-88.
Alammar N, Stein E. Irritable Bowel Syndrome: What Treatments Really Work. Med Clin North Am. enero de 2019;103(1):137-52.
Lacy BE, Pimentel M, Brenner DM, Chey WD, Keefer LA, Long MD, et al. ACG Clinical Guideline: Management of Irritable Bowel Syndrome. Am J Gastroenterol. 1 de enero de 2021;116(1):17-44.



