IBS-C and Stress: How Stress Affects Constipation in IBS
Understanding the relationship between IBS-C and stress can help improve symptom control and overall well-being.
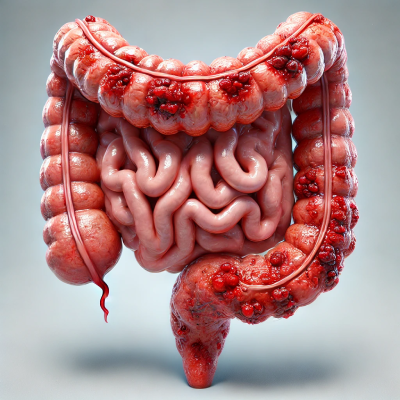
Irritable bowel syndrome with constipation (IBS-C) is a common digestive disorder that affects everyday life. Many people notice that their symptoms worsen in stressful situations.
Diagnosing IBS-C: Rome IV Criteria
The Rome IV criteria are the standardized guidelines used to diagnose C-IBS. According to these criteria, a person should experience recurrent abdominal pain at least once a week for the past three months, associated with at least two of the following:
- Changes in stool frequency.
- Relief or worsening of symptoms related to defecation.
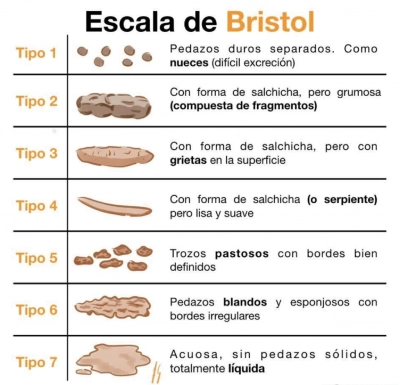
- Changes in stool form (more than 25% of stools classified as hard or lumpy according to the Bristol Scale type 1 and 2 and less than 25% as loose type 6 and 7).
These criteria help distinguish IBS-C from other gastrointestinal disorders and ensure accurate diagnosis for appropriate treatment.
The Relationship Between IBS-C and Stress
Stress plays an important role in IBS-C symptoms. The gut and brain are closely connected through the gut-brain axis, which means that emotional stress can directly affect bowel motility and sensitivity.
People with IBS-C often report that stressful situations trigger or worsen constipation, bloating and abdominal pain. Chronic stress can also affect the gut microbiota, leading to more digestive problems.
How stress worsens IBS-C symptoms:
- Slow digestion: Stress activates the body’s fight-or-flight response, diverting energy away from digestion and causing sluggish bowel movements.
- Increased intestinal sensitivity: Stress can make the intestines more reactive, intensifying discomfort and bloating.
- Alteration of the intestinal microbiota: Prolonged stress can negatively affect intestinal bacteria, which play a crucial role in digestion and regular bowel movements.
Strategies to Control IBS-C and Stress
Because of the relationship of IBS-C and stress as a trigger, managing it effectively can help improve symptoms. Here are some practical strategies:
- Mindfulness and relaxation techniques: Practicing meditation, yoga and deep breathing can help reduce stress levels and promote gut health.
- Regular exercise: Physical activity promotes digestion and helps manage stress, reducing IBS-C symptoms.
- Balanced diet: A diet rich in soluble fiber with adequate hydration promotes regular bowel movements. However, in some people, foods high in FODMAPs may worsen symptoms.
Remember to see a professional. Cognitive behavioral therapy (CBT) and gut-directed hypnotherapy have been shown to improve IBS symptoms by reducing stress and improving gut-brain communication.
Final Thoughts on IBS-C and Stress
In my experience as a nutritionist, recognizing the connection between IBS-C and stress is essential to managing symptoms effectively. Even if stress is not the cause of IBS-C, it can significantly worsen symptoms, so stress management is a key part of treatment.
By incorporating relaxation techniques, exercise and dietary adjustments, individuals can take control of their digestive health and improve their quality of life.

Written by: Nutritionist Andrés Izurieta
Bibliographic citations:
Schaper SJ, Stengel A. Emotional stress responsivity of patients with IBS – a systematic review. J Psychosom Res. 2022.
Kirkik D, Kalkanli Tas S. Unveiling the intricacies of irritable bowel syndrome. World J Gastroenterol. 2024.
Lacy BE, Pimentel M, Brenner DM, Chey WD, Keefer LA, Long MD, et al. ACG Clinical Guideline: Management of Irritable Bowel Syndrome. Am J Gastroenterol. 1 de enero de 2021;116(1):17-44.